F.M.S.
Fibromyalgia
Autoimmune diseases are on the rise. Both Fibromyalgia and Chronic Fatigue are autoimmune diseases. The fact is based upon new studies which show that immune tests are abnormal in both these conditions. Both of these diseases tend to occur in people who have other autoimmune diseases.
There are many ways to treat Fibromyalgia and Chronic Fatigue Syndrome here we are presenting the immunological features of these conditions. Where you can diagnose them by a blood tests and treat them by IVIg antibotics, electronic aids, vitamins, herbals or diet (see the diet page).
, herbals or diet (see the diet page).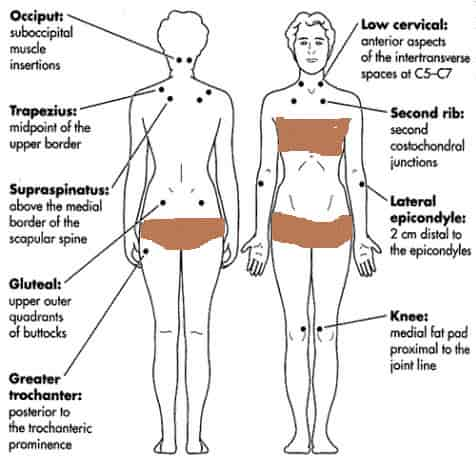
A person is supposed to have Fibromyalgia if they
have body pain in all or one half or all of the body for at least
six months. They have tender areas ito touch n the neck, back, hips,
shoulders, elbows and knees.. The pain usually gets worse when a
storm front is approaching and the barometer falls or early in the
morning. This is
associated with body stiffness worst in the morning. Pain usually tend to start on
the left side of the body with complaints of vague numbness. These
spells of numbness then spread to the other side of the body.eel
excessively tired. The fatigue is so severe that they have
difficulty doing things at home. Both Chronic Fatigue and
Fibromyalgia can occur in the same patient at the same time. With
chronic fatigue patients tend to have excessive infections like
sinusitis, flu, bronchitis or runny nose.
Fibromyalgia and Chronic Fatigue Syndrome are extremely common chronic condition . The current etiology is considered to be immune deficiency, characteristic alterations in the pattern of sleep and changes. The diagnosis is clinical and is characterized by widespread pain, tender points and, commonly, conditions such as chronic fatigue, sleep issues and depression. The diagnosis can be confirmed by doing a IgG and IgG sublass screen. Treatment is is by using IVIg, although experience and small clinical studies have proved the efficacy IVIg. Other less well-studied measures, such as trigger point treatment, also appear to be helpful. Management relies heavily on the physician's supportive counseling skills and willingness to try novel strategies in refractory cases described below.
Fibromyalgia is a immunologial neurological and rheumatologic condition characterized by spontaneous, widespread soft tissue pain, sleep disturbance, fatigue and extensively distributed areas of tenderness known as tender points. Estimates of prevalence are 3.4 percent for women and 0.5 percent for men.1
Pathophysiology
While the cause of fibromyalgia is currently considered by some to be a a immune mediated disease in some cases assossiated with a IgG subclass deficiency.
Fibromyalgia should be considered in any patient with musculoskeletal pain that is unrelated to a clearly defined anatomic lesion. Making the diagnosis of fibromyalgia depends on findings from the history and physical examination rather than on diagnostic testing.
In 1990, the American College of Rheumatology (ACR) established criteria for classifying patients with fibromyalgia.9 However, failure to meet these criteria does not absolutely exclude the possibility of fibromyalgia.
As with other rheumatologic disorders, fibromyalgia:
- Is established on the basis of clinical observations.
- Is a condition with signs and symptoms that exist on a continuum.
- Often requires observation over time to firmly establish the diagnosis.
- Some patients will have low IgG levels or low IgG subclass levels,
Widespread pain is characteristic of fibromyalgia. Although not all areas may be involved simultaneously, pain may occur in the occiput, neck, shoulders, thoracic and lumbar spine, paraspinous regions, buttocks, hips, elbows and knees. People complain of pain, knots and hearing noises when they move the neck or other joints. The complaints of numbness are vague and usually cross anatomic boundaries.
Continue to Fibromyalgia Physical Examination page
😏